View Providers

Immuno-oncology: Changing the Face of Cancer Research and Treatment
Immuno-oncology—sometimes better known as cancer
immunotherapy—is changing cancer care. Some patients whose prognoses were poor are
living longer and healthier lives than previously thought possible. But
immunotherapy isn’t a magic bullet, and it’s not appropriate for everyone with
cancer. Learning about immuno-oncology will help you when you talk with your
oncologist about your—or your loved one’s—treatment options.
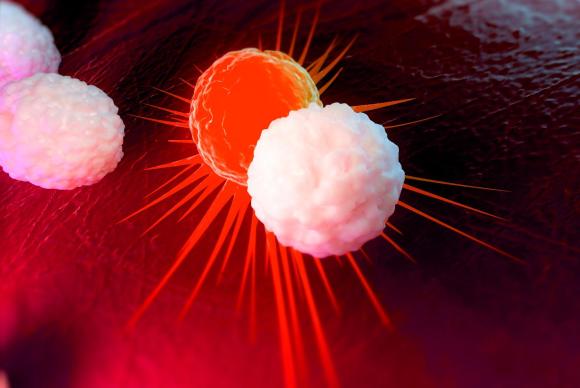
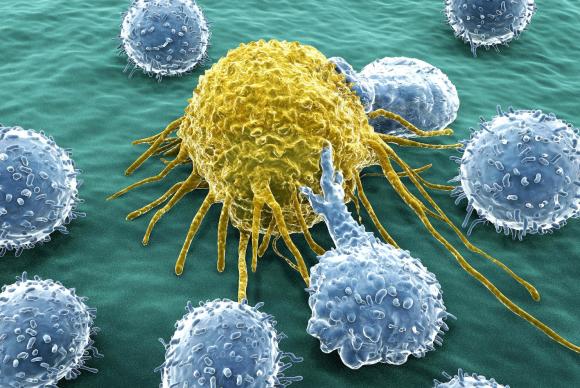
1. Immuno-oncology harnesses the immune system to treat cancer.
Traditional cancer treatments, including surgery,
chemotherapy and radiation, directly remove the cancerous tumor or kill cancer
cells. Immuno-oncology treatments stimulate the body’s immune system, so the
immune system attacks and destroys cancer cells. Immunotherapy treatments fall
into two categories: targeted immunotherapies
and general immunotherapies. Targeted
immunotherapies include cancer vaccines and so-called checkpoint inhibitors.
These medications help the immune system recognize and target cancer cells.
General immunotherapies boost the immune system and include interleukins and
interferons.

2. Cancer immunotherapy was named the 2016 Advance of the Year.
In 2016, immunotherapy drugs accounted for four of the 13
new anticancer treatments approved by the Food and Drug Administration (FDA),
and many more are under investigation. Doctors, scientists and patients are
really excited about immunotherapy because immunotherapy medications are
halting cancer in some patients—including patients whose cancer advanced
despite traditional treatment. Experts say immunotherapy has the potential to
transform cancer care, which is why the American Society of Clinical Oncology named
cancer immunotherapy the 2016 Advance of the Year.

3. Drugs based on immuno-oncology are now being used as a first treatment.
Immunotherapy was once only used when other treatments
failed to stop cancer growth. Keytruda (pembrolizumab) is the first
immunotherapy medication approved for use as a first-line treatment. The FDA
approved its use as a first treatment against non-small cell lung cancer that
has spread beyond the lungs because clinical studies showed Keytruda was more
effective (and better tolerated by the patient) than standard chemotherapy.
Researchers are currently investigating whether or not immunotherapy might be
an effective first treatment for other types of cancer as well.

4. Immunotherapy is approved to treat lymphoma, lung, kidney, skin and head and neck cancers.
The current revolution in immunotherapy began when Keytruda
and Opdivo (nivolumab) were approved to treat melanoma, a deadly form of skin
cancer, in 2014. Since then, the FDA has approved immunotherapy medications to
treat lymphoma, non-small cell lung cancer, renal cell carcinoma (a form of
kidney cancer), bladder cancer, and head and neck cancers. Researchers suspect
immunotherapy will be effective against other types of cancers as well. They
are actively studying how various cancers respond to these medications.

5. Immuno-oncology doesn’t benefit all cancer patients.
The results of immuno-oncology treatment can be impressive.
Some patients with advanced cancer are living years longer than would be
normally expected, and some have no evidence of disease after treatment.
However, those patients are in the minority. Only about 15 to 30% of patients
see their cancer shrink or vanish with treatment. Researchers are currently
trying to untangle why some people respond and others don’t, and are developing
tests to predict whether or not a patient will benefit from immuno-oncology.

6. Most patients tolerate immuno-oncology drugs better than traditional cancer treatments.
According to at least one research study, patients who
received immunotherapy to treat lung cancer experienced fewer side effects than
patients who received chemotherapy. They reported an improved quality of life
too; compared to their peers receiving chemotherapy, the patients receiving
immunotherapy were better able to function physically, emotionally and
socially. The most common immunotherapy side effects include fever, chills, fatigue,
nausea, and skin reactions where the medicine enters the body. Other side
effects include diarrhea, fluid retention, headache, heart palpitations, and
sinus congestion.

7. Potentially serious side effects are possible.
Although serious side effects are rare, immuno-oncology
treatments can cause lung inflammation, rheumatoid arthritis, and colitis, an
inflammation of the intestine that causes diarrhea and can be fatal.
Immunotherapy drugs can also affect the thyroid, adrenal and pituitary glands,
which secrete important hormones. Your care team will closely monitor you for
side effects. It is important to tell your doctor about any new or a change in
symptoms you experience, especially difficulty breathing or changes in bowel
habits. Doctors may need to adjust or stop your medication. Other medicines may
be an option to control side effects.

8. Immuno-oncology is giving patients and families hope.
One reason healthcare providers, patients and families are
so excited about immuno-oncology is that immunotherapy treatments give patients
hope for life after cancer. Currently, over half of people diagnosed with lung
cancer die within a year of diagnosis, and just 18% of patients are alive five
years after diagnosis. But with immunotherapy, some patients whose cancer
progressed despite surgery, chemotherapy and radiation are still alive and
healthy.
9. Hundreds of immuno-oncology clinical trials are currently under way.
Researchers are testing new immunotherapy medications and
comparing the effect with chemotherapy drugs to see which treatment works
better for certain cancers. They are also testing how well immunotherapy works when
administered with chemotherapy and radiation. Those tests are essential for
cancer specialists to know which treatment to use first and if a particular combination
of therapies delivers optimal outcomes. Your healthcare provider can help you
determine if you’re eligible for an immuno-oncology clinical trial.



